
-François Grolleau-
Anesthesiology and Critical Care physician
Postdoctoral Scholar at
Stanford Center for Biomedical Informatics Research
with Prof. Jonathan Chen

Anesthesiology and Critical Care physician
Postdoctoral Scholar at
Stanford Center for Biomedical Informatics Research
with Prof. Jonathan Chen
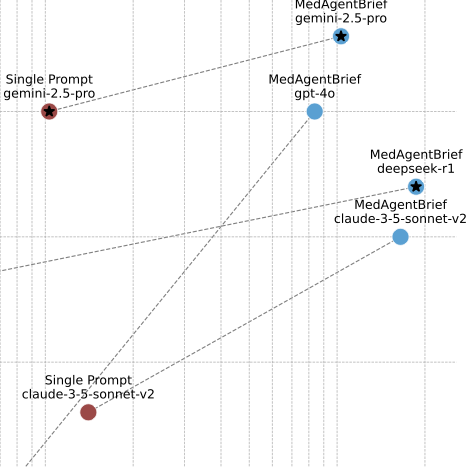
MedFactEval is a clinician-grounded framework where key facts are defined by physicians and an LLM jury checks whether AI drafts include or contradict them. MedAgentBrief is a model-agnostic, stepwise workflow that builds discharge summaries with traceable links back to the source notes. The MedAgentBrief pipeline is now deployed at Stanford’s Sequoia hospital, where physicians use it as the first draft of their discharge summaries.
We introduce powerROC, an open-source web tool designed to simplify sample size calculations for AUROC-based external validation studies. We review key concepts for accurate sample size determination, making the theory and practice more accessible to researchers and clinicians. The tool supports evaluating a single model and comparing two models, with guidance on selecting target precision levels using pilot data or user-defined probability distributions.
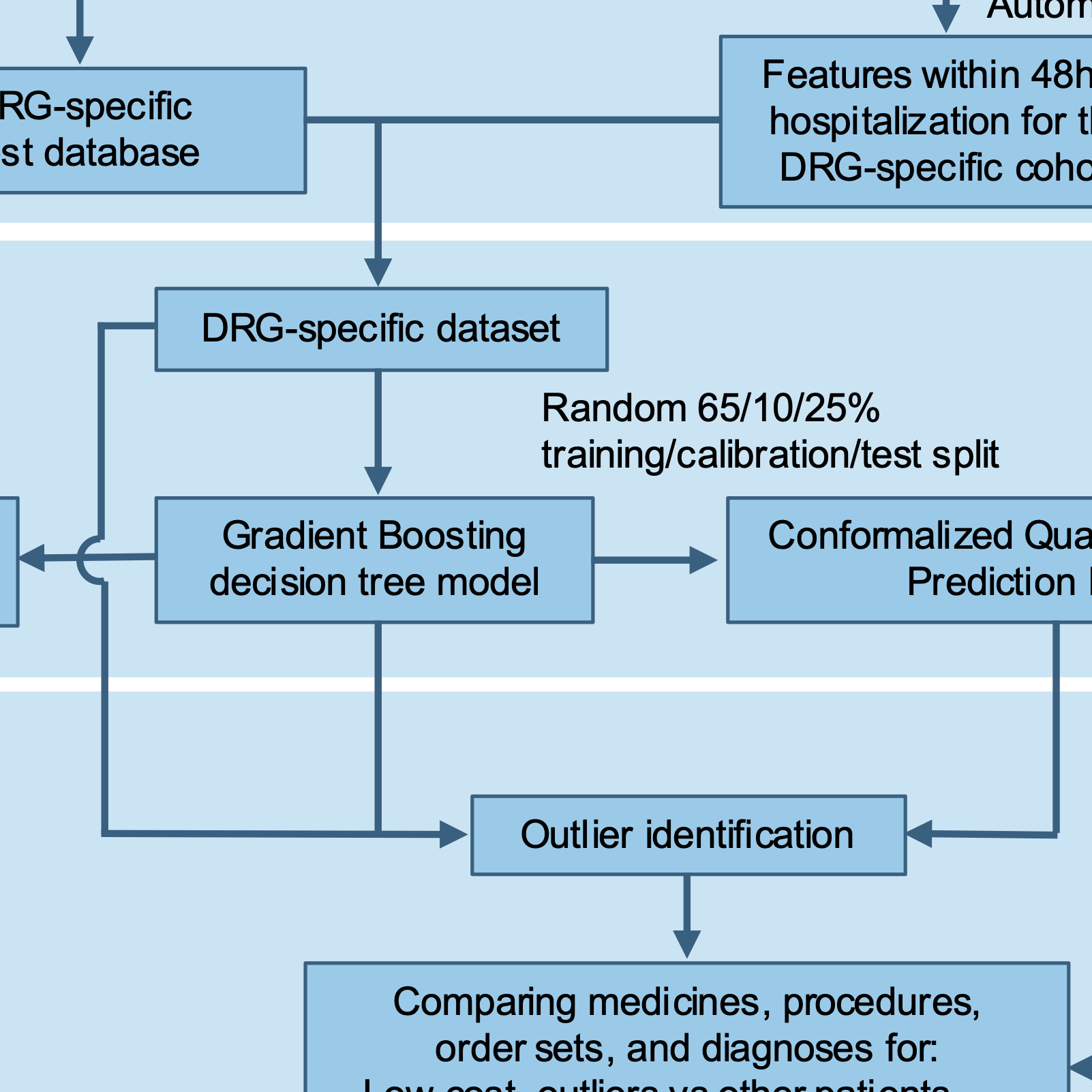
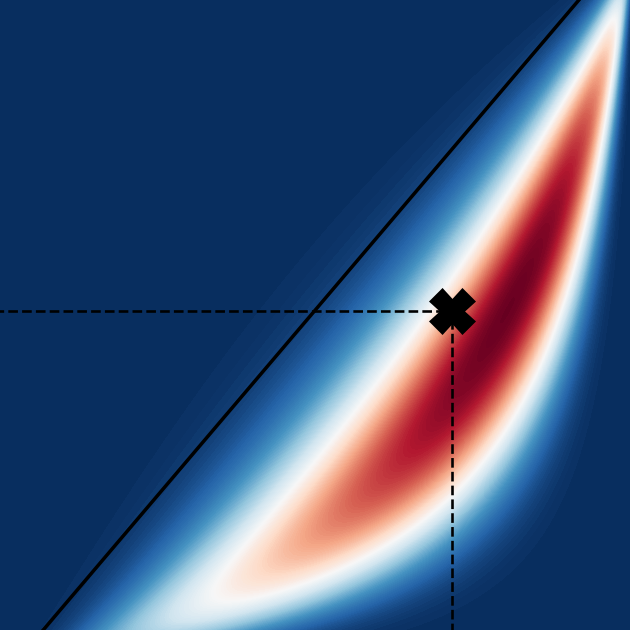
We introduce a novel outlier detection method for Electronic Health Records using Conformal Prediction to address hospital cost variability. This approach employs Conformal Quantile Regression to generate robust prediction intervals, providing a comprehensive view of cost variability. By integrating this method with machine learning models, healthcare professionals can identify opportunities for quality and efficiency improvements in clinical practices.
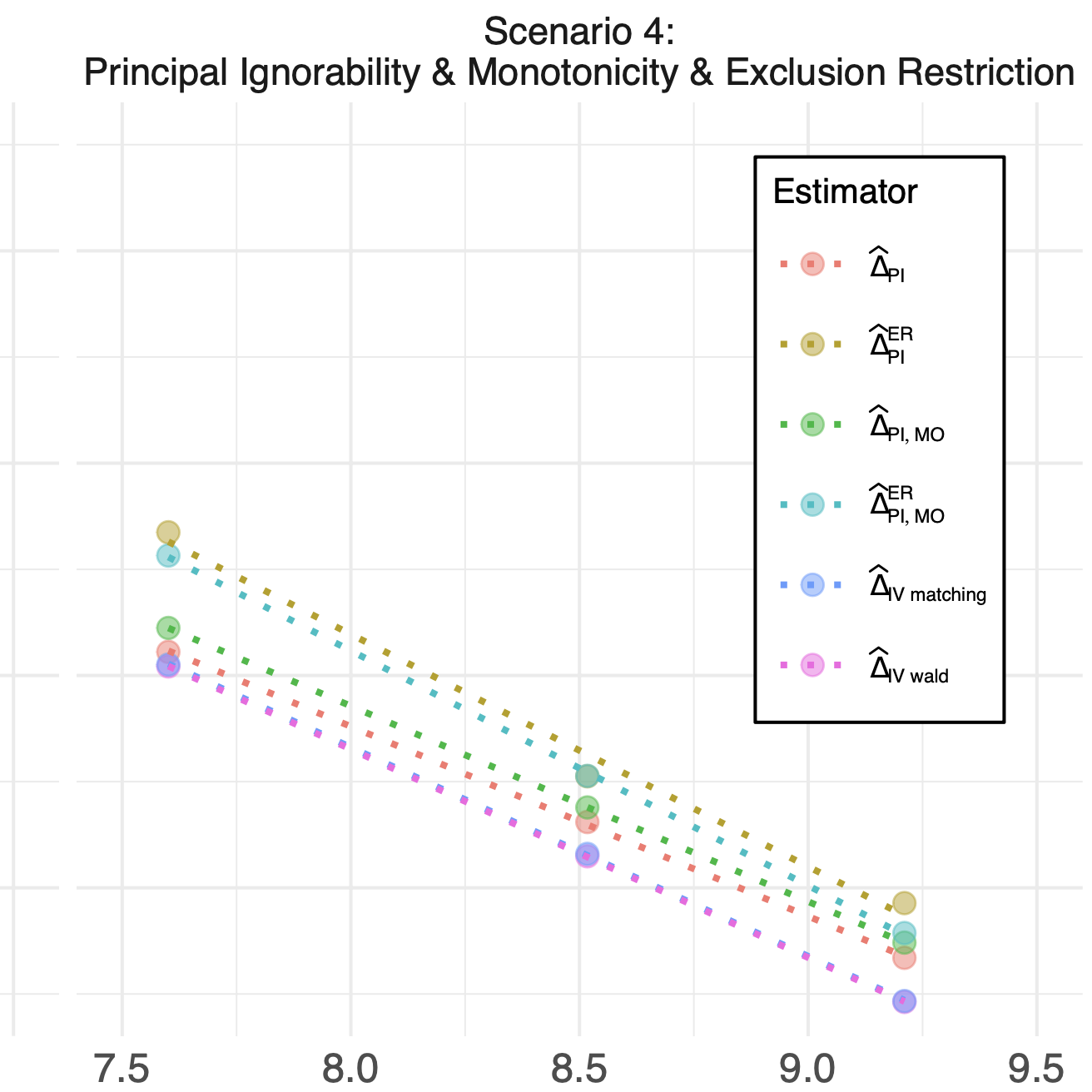
In healthcare, it’s essential to evaluate the effects of medical interventions. We introduced a new technique to estimate the Complier Average Causal Effect (CACE) without depending on problematic assumptions such as exclusion restriction and monotonicity. We examined the theoretical properties of our approach and demonstrate its performance and applicability in both simulated and real-world scenarios.
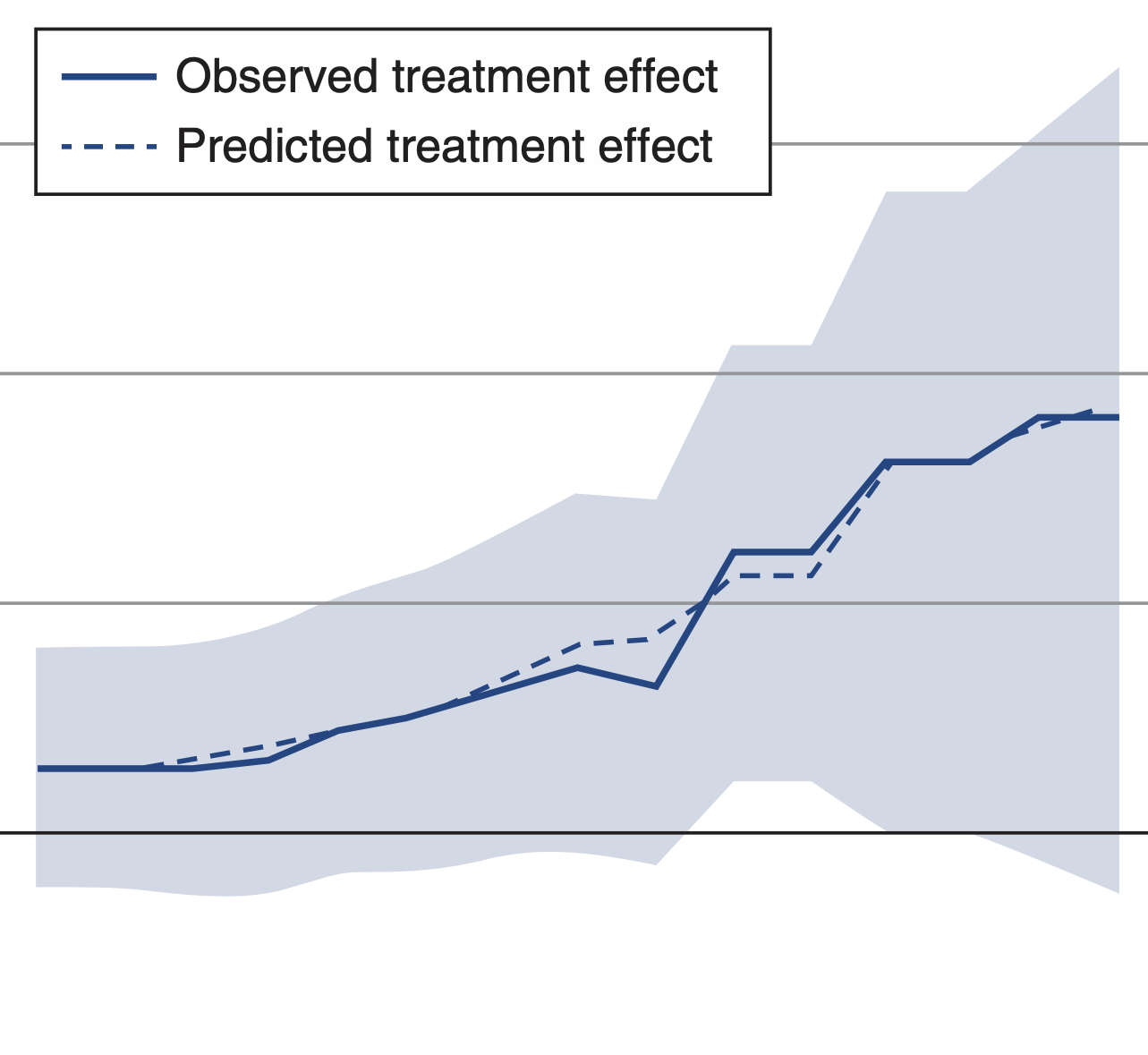
We developed and externally validated a dynamic renal replacement therapy initiation strategy for ICU patients with severe acute kidney injury. Our study suggests that implementing this new individualized strategy could increase the average number of days ICU patients spend alive and outside the hospital. We further found that the implementation could help save health resources all the while reducing unnecessary treatment burdens.
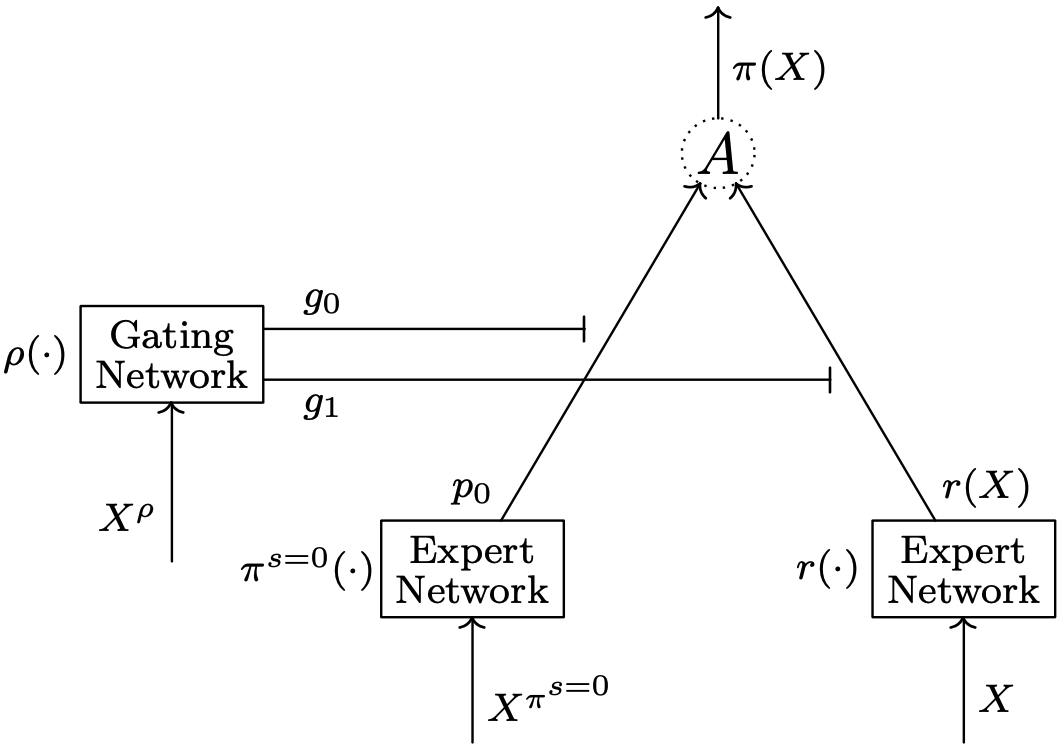
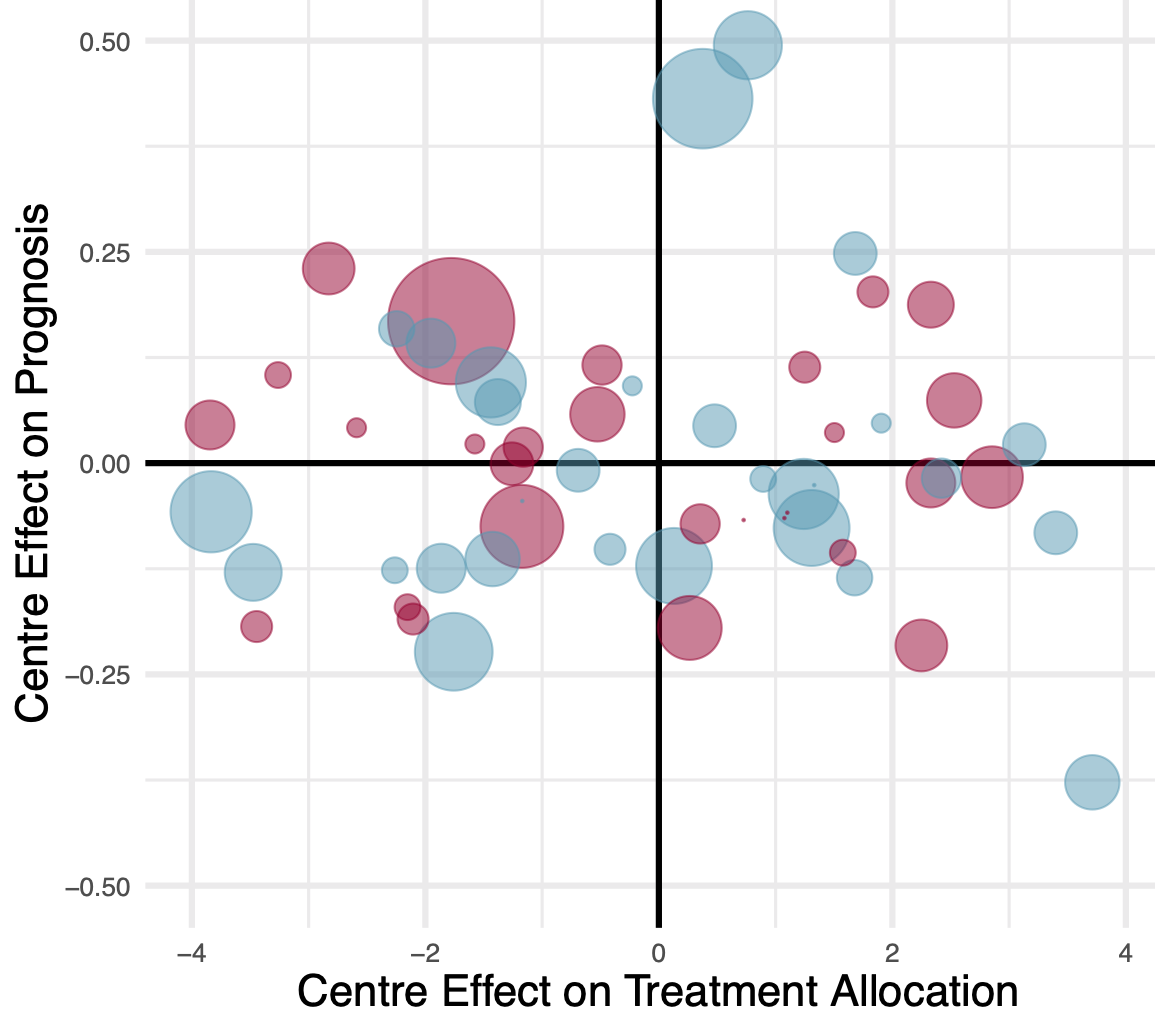
Individualized treatment rules are deterministic decision rules that recommend treatments to individuals based on their characteristics. Though ubiquitous in medicine, individualized treatment rules are hardly ever evaluated in randomized controlled trials. To evaluate individualized treatment rules from observational data, we introduce a new probabilistic model and propose an estimation procedure that relies on an expectation-maximization algorithm. We illustrate our approach on the MIMIC-III database.
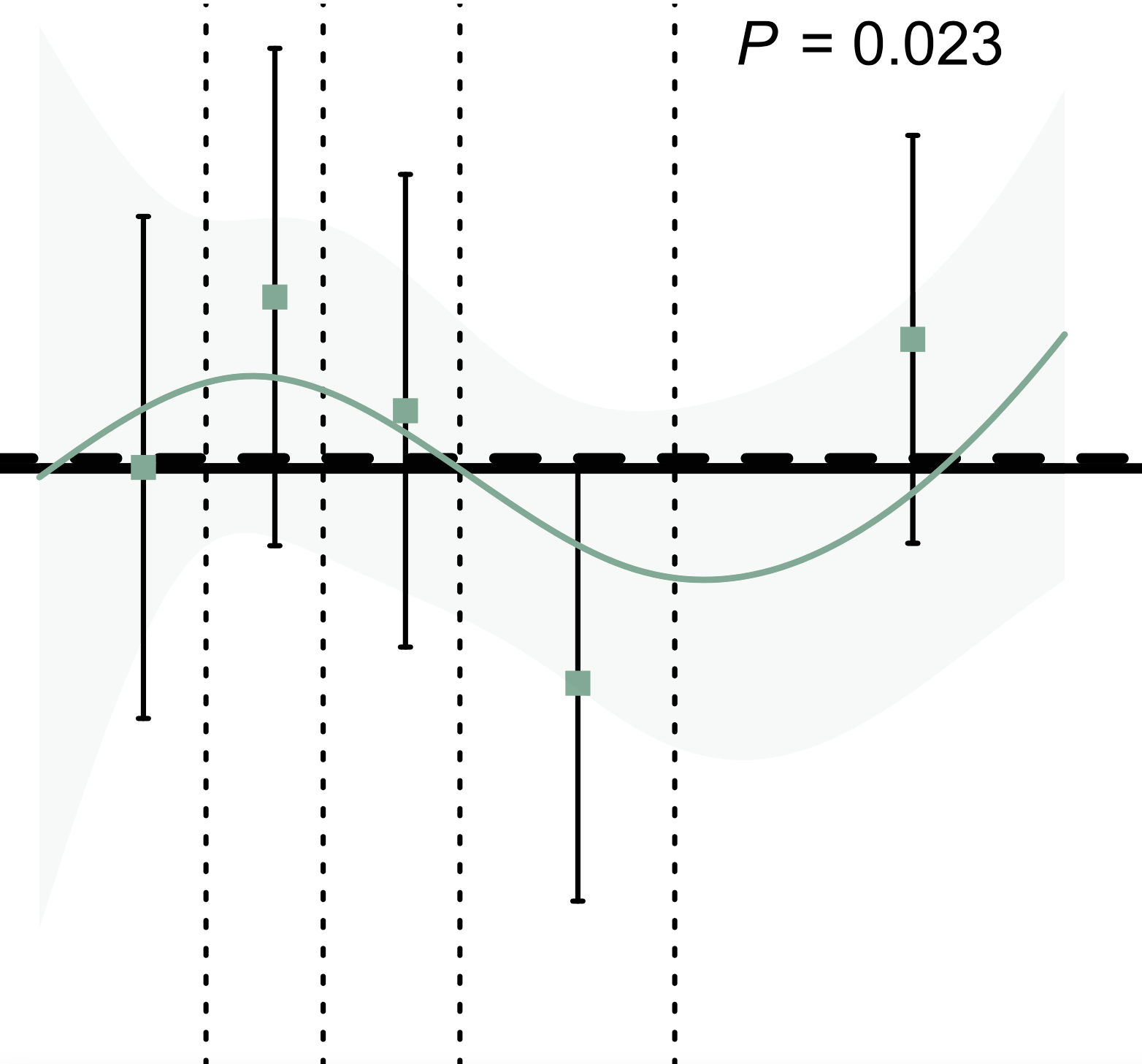
Randomized trials comparing early and delayed strategies of renal replacement therapy in patients with severe acute kidney injury may have missed differences in survival as a result of mixing patients at heterogeneous levels of baseline risk. Using data from the AKIKI and IDEAL‐ICU trials, we identified a heterogeneity of treatment effects from an early vs a delayed strategy across levels of risks. This heterogeneity in survival may reflect varying degrees of kidney demand‐capacity mismatch.
Recent results from the PEXIVAS trial challenged the role of plasma exchange in ANCA-associated vasculitis. We aimed to evaluate whether histopathologic findings could predict kidney function and help identify which patients would most benefit from plasma exchanges. We developed a scoring system to identify the subset of patients who would benefit from plasma exchange.
Intermittent hemodialysis and continuous renal replacement therapy are the main renal replacement therapy modalities for patients with severe acute kidney injury. Following the emulated target trial principle, we reanalyzed data from AKIKI and IDEAL-ICU to evaluate which of these two modalities best improved patients-important outcomes. Compared to intermittent hemodialysis, we found no evidence that continuous renal replacement therapy improved survival or kidney recovery; however, we noted that intermittent hemodialysis may be a better choice in patients with lesser severity of the disease.
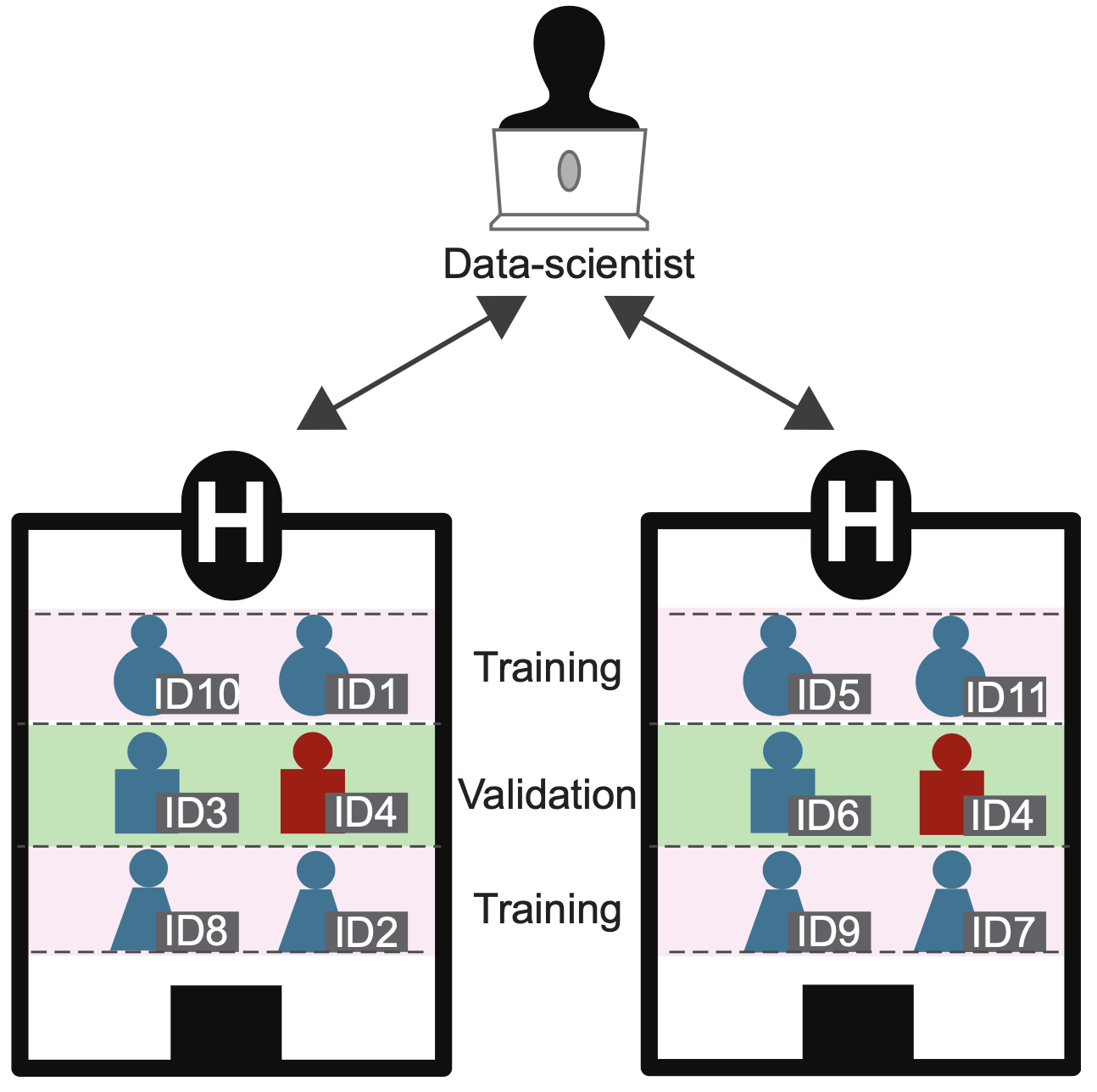
We introduce a validation methodology compatible with privacy-preserving federated learning that prevents data leakage caused by duplicates of electronic health records. We perform Monte Carlo simulations to investigate the properties of our procedure—in the case of the validation of a predictive gradient boosting model. We further illustrate this on MIMIC-III medical records and show that when a covariate weakly associated with the outcome is available on duplicated records, our approach prevents overoptimistic estimations of accuracy.
In anesthesia and critical care, most trials are single-center with negative findings. In this work, we focused on the studies with positive findings and evaluated their result’s robustness with a new statistical metric—the Fragility Index. We found that the results of anesthesia and critical care trials with statistically significant findings are often fragile and that articles’ conclusions were frequently affected by spin.